Literacy Crisis: Health Education to Increase Public Awareness of Clinical Communication in the Digital Age
https://doi.org/10.51574/ijrer.v4i3.3547
Keywords:
Clinical Communication, Digital Age, Health Education, Health LiteracyAbstract
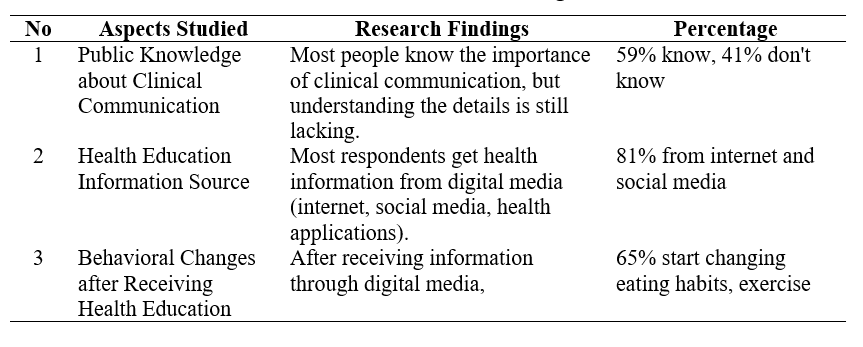
The background of this study began with the low level of health literacy, which has an impact on patients' understanding of technical terms during medical consultations. With the rapid development of information technology, people now find it easier to access various health information through digital media but are also faced with challenges related to filtering accurate and reliable information. Health education is an important factor in guiding people to understand and implement a healthy lifestyle based on correct information. Therefore, this study aims to analyze the role of health education in increasing public awareness of clinical communication in the digital era. In addition, it examines the phenomenon of patient confusion regarding medical terminology in clinical communication practices. Using a qualitative descriptive approach, researchers conducted in-depth interviews with eight patients aged 25–60 years, all of whom did not have a medical education background. The Wami Jaya Health Center in Nabire Regency conducted this study. Data were analyzed thematically. The results of the study showed that, although most people are used to accessing health information online, there are still gaps in understanding and implementing appropriate clinical communication. Therefore, health education programs that utilize digital technology, such as webinars, health applications, and interactive educational content, can be an effective solution to increase public awareness and knowledge about clinical communication. In addition, the research findings revealed four main patterns: lack of understanding of medical terms, passive communication behavior, linguistic gaps between doctors and patients, and ineffectiveness of written educational materials. This study concludes that the health literacy crisis is not just an individual problem but also a reflection of an unresponsive communication system.
References
Ahmed, S. K. (2024). The pillars of trustworthiness in qualitative research. Journal of Medicine, Surgery, and Public Health, 2, 100051. https://doi.org/10.1016/j.glmedi.2024.100051
Anisah, N., Sartika, M., & Kurniawan, H. (2021). Penggunaan media sosial Instagram dalam meningkatkan literasi kesehatan pada mahasiswa. Jurnal Peurawi: Media Kajian Komunikasi Islam, 4(2), 94-112. https://doi.org/10.22373/jp.v4i2.11080
Anwar, R. K., Khadijah, U. L. S., & Rizal, E. (2023). Instagram and Digital Media Literacy among Teenagers in Bandung. Communicatus: Jurnal Ilmu Komunikasi, 7(2), 123-142. https://doi.org/10.15575/cjik.v7i2.23640
Baumeister, A., Chakraverty, D., Aldin, A., Seven, Ü. S., Skoetz, N., Kalbe, E., & Woopen, C. (2021). “The system has to be health literate, too”-perspectives among healthcare professionals on health literacy in transcultural treatment settings. BMC Health Services Research, 21, 1-16. https://doi.org/10.1186/s12913-021-06614-x
Boulos, M. N. K., Hetherington, L., & Wheeler, S. (2007). Second Life: an overview of the potential of 3‐D virtual worlds in medical and health education. Health Information & Libraries Journal, 24(4), 233-245. https://doi.org/10.1111/j.1471-1842.2007.00733.x
Brach, C., & Harris, L. M. (2021). Healthy people 2030 health literacy definition tells organizations: make information and services easy to find, understand, and use. Journal of general internal medicine, 36(4), 1084-1085. https://doi.org/10.1007/s11606-020-06384-y
Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11(4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
Creswell, J. W., & Poth, C. N. (2016). Qualitative inquiry and research design: Choosing among five approaches. Sage publications.
Dąbrowska, J., Almpanopoulou, A., Brem, A., Chesbrough, H., Cucino, V., Di Minin, A., ... & Ritala, P. (2022). Digital transformation, for better or worse: a critical multi‐level research agenda. R&D Management, 52(5), 930-954. https://doi.org/10.1111/radm.12531
de Vasconcelos, P. F., de Freitas, C. H. A., Jorge, M. S. B., de Carvalho, R. E. F., de Sousa Freire, V. E. C., de Araújo, M. F. M., ... & Oliveira, A. C. S. (2019). Safety attributes in primary care: understanding the needs of patients, health professionals, and managers. Public health, 171, 31-40. https://doi.org/10.1016/j.puhe.2019.03.021
Durowaye, T. D., Rice, A. R., Konkle, A. T., & Phillips, K. P. (2022). Public health perinatal promotion during COVID-19 pandemic: a social media analysis. BMC public health, 22(1), 895. https://doi.org/10.1186/s12889-022-13324-4
Easton, P., Entwistle, V. A., & Williams, B. (2013). How the stigma of low literacy can impair patient-professional spoken interactions and affect health: insights from a qualitative investigation. BMC health services research, 13, 1-12. https://doi.org/10.1186/1472-6963-13-319
Ghahramani, A., de Courten, M., & Prokofieva, M. (2022). The potential of social media in health promotion beyond creating awareness: an integrative review. BMC public health, 22(1), 2402. https://doi.org/10.1186/s12889-022-14885-0
Hannawa, A. F., Wu, A. W., Kolyada, A., Potemkina, A., & Donaldson, L. J. (2022). The aspects of healthcare quality that are important to health professionals and patients: A qualitative study. Patient education and counseling, 105(6), 1561-1570. https://doi.org/10.1016/j.pec.2021.10.016
Hasibuan, A. R., Pasaribu, A. F., Alfiyah, S., Utami, J. N., & Harahap, N. R. Y. (2024). Peran Pendidikan Kesehatan dalam Meningkatkan Kesadaran Masyarakat Terhadap Pola Hidup Sehat di Era Digital. Didaktika: Jurnal Kependidikan, 13(001 Des), 305-318. https://doi.org/10.58230/27454312.1515
Li, C., Liu, M., Zhou, J., Zhang, M., Liu, H., Wu, Y., ... & Deng, T. (2022). Do health information sources influence health literacy among older adults: a cross-sectional study in the urban areas of western China. International journal of environmental research and public health, 19(20), 13106. https://doi.org/10.3390/ijerph192013106
Lin, A. (2013). Citizenship education in American schools and its role in developing civic engagement: a review of the research. Educational Review, 67(1), 35–63. https://doi.org/10.1080/00131911.2013.813440
Mazzi, M. A., Rimondini, M., Deveugele, M., Zimmermann, C., Moretti, F., Van Vliet, L., ... & Bensing, J. (2015). What do people appreciate in physicians' communication? An international study with focus groups using videotaped medical consultations. Health Expectations, 18(5), 1215-1226. https://doi.org/10.1111/hex.12097
Melchior, C., & Oliveira, M. (2022). Health-related fake news on social media platforms: A systematic literature review. New Media & Society, 24(6), 1500-1522. https://doi.org/10.1177/14614448211038762
Nutbeam, D. (2019). Health education and health promotion revisited. Health Education Journal, 78(6), 705-709. https://doi.org/10.1177/0017896918770215
Patel, V. L., Yoskowitz, N. A., Arocha, J. F., & Shortliffe, E. H. (2009). Cognitive and learning sciences in biomedical and health instructional design: A review with lessons for biomedical informatics education. Journal of biomedical informatics, 42(1), 176-197. https://doi.org/10.1016/j.jbi.2008.12.002
Paul, J., Ueno, A., Dennis, C., Alamanos, E., Curtis, L., Foroudi, P., ... & Wirtz, J. (2024). Digital transformation: A multidisciplinary perspective and future research agenda. International Journal of Consumer Studies, 48(2), e13015. https://doi.org/10.1111/ijcs.13015
Pawlikowska, T., Zhang, W., Griffiths, F., Van Dalen, J., & van der Vleuten, C. (2012). Verbal and non-verbal behavior of doctors and patients in primary care consultations–How this relates to patient enablement. Patient education and counseling, 86(1), 70-76. https://doi.org/10.1016/j.pec.2011.04.019
Petretto, D. R., Carrogu, G. P., Gaviano, L., Berti, R., Pinna, M., Petretto, A. D., & Pili, R. (2024). Telemedicine, e-health, and digital health equity: a scoping review. Clinical practice and epidemiology in mental health: CP & EMH, 20, e17450179279732. https://doi.org/10.2174/0117450179279732231211110248
Sahroni, S., Anshari, D., & Krianto, T. (2019). Social Determinants of the Level of Health Literacy in Hypertension Patients in the Public Health Center of the Cilegon City. Faletehan Health Journal, 6(3), 111-117. https://doi.org/10.33746/fhj.v6i3.94
Sætra, H. S., & Fosch-Villaronga, E. (2021). Healthcare digitalisation and the changing nature of work and society. In Healthcare (Vol. 9, No. 8, p. 1007). MDPI. https://doi.org/10.3390/healthcare9081007
Seibert, R. G., Winter, M. R., Cabral, H. J., Wolf, M. S., Curtis, L. M., & Paasche-Orlow, M. K. (2019). Health literacy and income mediate racial/ethnic asthma disparities. HLRP: Health Literacy Research and Practice, 3(1), e9-e18. https://doi.org/10.3928/24748307-20181113-01
Shan, R., Sarkar, S., & Martin, S. S. (2019). Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia, 62(6), 877-887. https://doi.org/10.1007/s00125-019-4864-7
Sharma, M. (2021). Theoretical foundations of health education and health promotion. Jones & Bartlett Learning.
Sørensen, K. (2024). Fostering digital health literacy to enhance trust and improve health outcomes. Computer Methods and Programs in Biomedicine Update, 5, 100140. https://doi.org/10.1016/j.cmpbup.2024.100140
Sørensen, K., Pelikan, J. M., Röthlin, F., Ganahl, K., Slonska, Z., Doyle, G., ... & Brand, H. (2015). Health literacy in Europe: Comparative results of the European Health Literacy Survey (HLS-EU). European Journal of Public Health, 25(6), 1053–1058. https://doi.org/10.1093/eurpub/ckv043
Stellefson, M., Paige, S. R., Chaney, B. H., & Chaney, J. D. (2020). Evolving role of social media in health promotion: updated responsibilities for health education specialists. International journal of environmental research and public health, 17(4), 1153. https://doi.org/10.3390/ijerph17041153
Stoumpos, A. I., Kitsios, F., & Talias, M. A. (2023). Digital transformation in healthcare: technology acceptance and its applications. International journal of environmental research and public health, 20(4), 3407. https://doi.org/10.3390/ijerph20043407
Taba, M., Allen, T. B., Caldwell, P. H., Skinner, S. R., Kang, M., McCaffery, K., & Scott, K. M. (2022). Adolescents’ self-efficacy and digital health literacy: a cross-sectional mixed methods study. BMC Public Health, 22(1), 1223. https://doi.org/10.1186/s12889-022-13599-7
Taylan, C., & Weber, L. T. (2023). “Don’t let me be misunderstood”: communication with patients from a different cultural background. Pediatric Nephrology, 38(3), 643-649. https://doi.org/10.1007/s00467-022-05573-7
Tyagi, R., Vishwakarma, S., Rishi, M., & Rajiah, S. (2021). Reducing inequalities through education and skill development courses. In Reduced Inequalities (pp. 746-758). Cham: Springer International Publishing. https://doi.org/10.1007/978-3-319-95882-8_102
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Winda Woro Mahmudah, Ronggo Santoso

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.